Virtual Care is entering a new era that promises tremendous benefits to patients and healthcare providers alike. During the COVID-19 pandemic, the telehealth field made huge advances. This growth occurred so quickly that concepts recently thought of as cutting-edge are now commonplace.
Here’s a look at how video visits with healthcare providers are markedly different from comprehensive Virtual Care services.
Virtual Care: What Happens Beyond the Video
During the pandemic, many leaders in the healthcare field adopted telehealth as an emergency measure. That was smart because serving patient needs was crucial and with the regulations lifted, two-way video conferencing quickly met immediate requirements to safely engage and deliver patient care.
With some normalcy now returned, healthcare organizations are learning that their move to a videoconferencing-only solution isn’t enough. Whether you choose Teams, Zoom, FaceTime, or Google-Meet to deliver remote patient care via video visits, you learned a lot through the past 18 months. Top among these learnings is that two-way video solutions don’t have the many dynamic features of an end-to-end Virtual Care solution.
There are many differences between video visits and Virtual Care.
Virtual Care is a comprehensive set of end-to-end capabilities to enable remote care delivery. Video visits are just one stage in the overall Virtual Care process. Virtual Care virtualizes every step in the patient’s journey: scheduling, intake, care coordination, the video visit itself, ePrescribe, and discharge, including sophisticated reporting and analytics. Virtual Care has the power to reduce friction points, enhance clinical workflows, while improving patient outcomes, reducing costs, and boosting revenue.
The Cost of a Fragmented Process
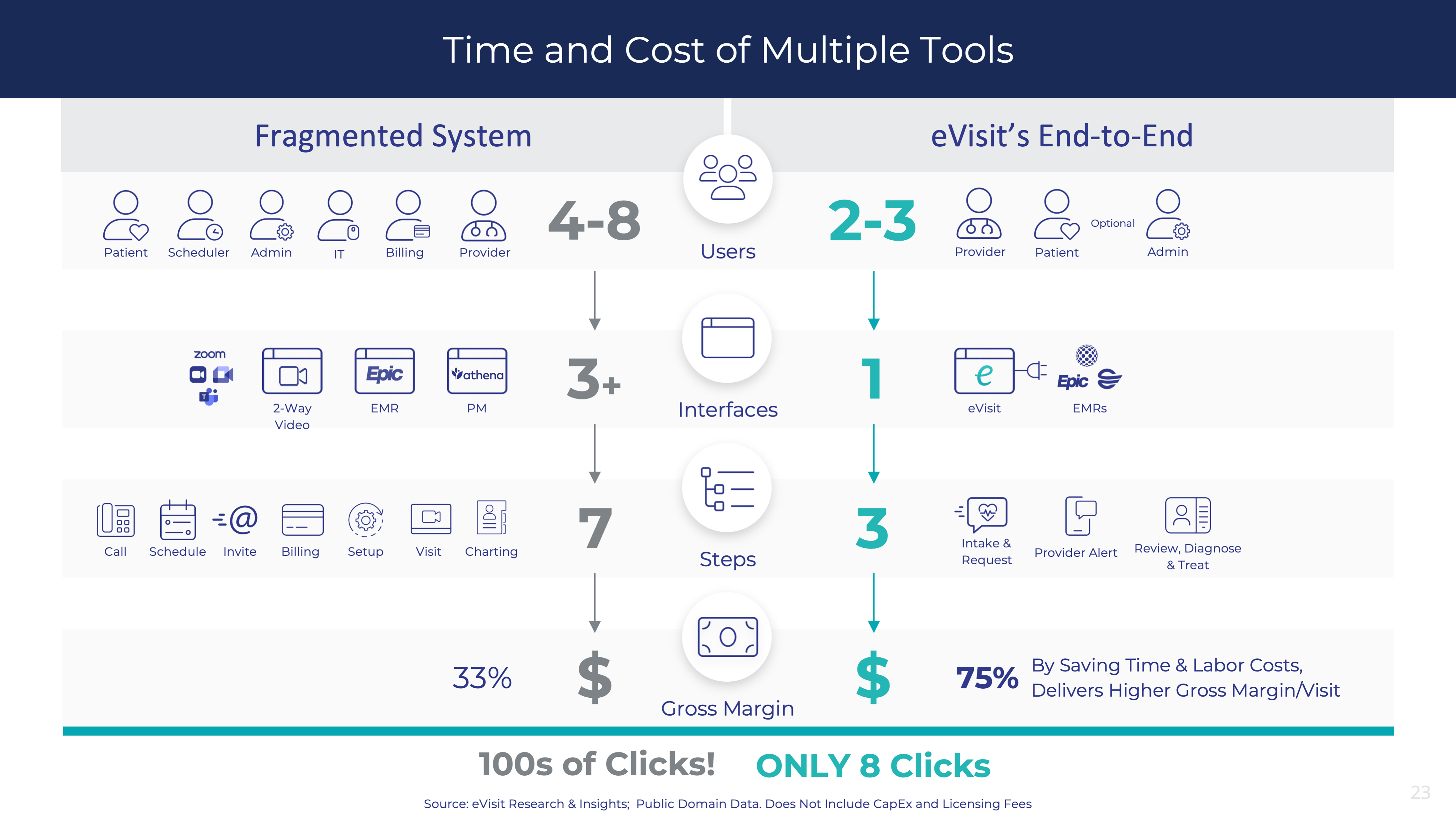
The eVisit Research & Insights Team has studied the differences, and the business impact, between video visits and Virtual Care. The above infographic details the significant disparity, especially the many friction points HCOs encounter as they marry the myriad of “non-virtualized” physical steps — and the many team members — it takes to conduct a single video visit for just one patient.
These non-virtualized steps actually take as many as eight practice team members to navigate and transact the video visit process. With video visits, there are multiple software and interfaces in play including the practice management suite, Electronic Health Record (EHR) system and two-way video system and many team members who are phoning, emailing, texting, diagnosing, adjudicating, billing, charting and prescribing.
An end-to-end unified platform that virtualizes every step in the clinical workflow process lets the provider — flying solo or aided by an admin staff member — deliver patient care from start-to-finish. The patient can self-serve along the way with a superior and easy-to-use user experience.
Ultimately, a video visit entails 133% more steps, hundreds of clicks and more labor hours. Our studies show that using an end-to-end solution like eVisit saves time and labor costs and delivers a higher gross margin per visit: 75% vs. 33% with a two-way video visit solution.
The Five Critical Capabilities for Virtual Care Solutions
Gartner’s “2020 Market Guide for Virtual Care Solutions,” in which eVisit is one of 20 Representative Vendors, calls for Virtual Care to demonstrate five critical capabilities.
- Simplified and seamless integration. To maximize revenue and efficiency, it is critical for healthcare providers to have tight integration of Virtual Care within clinical workflows.
- Frictionless patient and consumer experience. This will be a key critical success factor as healthcare providers seek to sustain and scale Virtual Care services beyond the COVID-19 pandemic.
- Artificial intelligence driving clinical efficacy and efficiency. This, too, will be a fundamental differentiator in optimizing clinical encounters and maximizing efficiency.
- Information capture for billing and protection against fraud. The ability to accurately capture and report on clinical activity, as well as appropriately verify and identify patients, will be essential to the staying power of Virtual Care. Governments and healthcare payers across the world are beginning to move from temporary Virtual Care funding arrangements to permanent agreements.
- Modular, open solutions for composable experiences. Healthcare providers will need flexibility to adapt to changing requirements in the Virtual Care space, while leveraging existing investments simultaneously. Thus, there will be the need for Virtual Care solutions that are both modular and open—in other words, easily adaptable.
Health providers are to be commended for the way they developed video visit capabilities during the pandemic. The clear direction of the market is building on that momentum and moving toward system-wide Virtual Care services that can enhance clinical efficiencies and profits, as well as patient outcomes.
Click the button below to learn more about the eVisit Virtual Care platform and our Virtual Care Maturity Model™ from our team of Virtual Care Consultants. Learn more at eVisit.com.