What is Telemedicine?
Learn about this rapidly expanding field in our definitive guide.
Telemedicine is a relatively new concept, and in the world of internet, it develops with lightning speed. This article is for those who want to understand all intricacies of this highly dynamic and fascinating field.
Table of Content:
- History of Telemedicine
- Telemedicine Today
- The Difference Between Telemedicine and Telehealth
- Telemedicine Pros and Cons
- Top Telemedicine Medical Specialties
- What services can be provided by telemedicine
- How Telemedicine Can be Used
- Types of Telemedicine
- Telemedicine Clinical Guidelines
- Telemedicine and Medicare
- Telemedicine and Medicaid
- Future of Telemedicine
- Telemedicine Statistics
- Telehealth Resource Centers
- Telemedicine Regulations
- Barriers to Telemedicine
- Who Pays for Telemedicine
- HIPAA and Telemedicine
- Telemedicine Terms
1. History of Telemedicine
The field of telemedicine has changed drastically from its inception. It was only about fifty years ago that a few hospitals started experimenting with telemedicine to reach patients in remote locations. But with the rapid changes in technology over the last few decades, telemedicine has transformed into a complex integrated service used in hospitals, homes, private physician offices, and other healthcare facilities.
The concept of telemedicine started with the birth of telecommunications technology, the means of sending information over a distance in the form of electromagnetic signals. Early forms of telecommunications technology included the telegraph, radio, and telephone. In the late 19th century, the radio and telephone were just starting to emerge as viable communication technologies. Alexander Graham Bell patented the telephone in 1876 and Heinrich Rudolf Hertz performed the first radio transmission in 1887.
But it wasn’t until the early 20th century that the general population started to these technologies, and imagine they could be applied to the field of medicine. In 1925, a cover illustration of the Science and Invention magazine featured an odd invention by Dr. Hugo Gernsback, called the “teledactyl.” The imagined tool would use spindly robot fingers and radio technology to examine a patient from afar, and show the doctor a video feed of the patient. While this invention never got past the concept stage, it predicted the popular telemedicine definition we think of today – a remote video consult between doctor and patient.
Several decades later, in the 1950’s, a few hospital systems and university-based medical centers experimenting with how to put concept of telemedicine into practice. Medical staff at two different health centers in Pennsylvania about 24 miles apart transmitted radiologic images via telephone. In 1950’s, a Canadian doctor built upon this technology into a Teleradiology system that was used in and around Montreal. Then, in 1959, Doctors at the University of Nebraska were able to transmit neurological examinations to medical students across campus via a two-way interactive television. By 1964, they had built a telemedicine link that allowed them to provide health services at Norfolk State Hospital, 112 miles away from campus.
Originally, health professionals developed this technology to reach remote patients living in the rural areas. But with time, medical staff and the U.S. government saw the big picture – the potential to reach urban populations with healthcare shortages, and to respond to medical emergencies by sharing medical consults and patient health records without delay. In the 1960s, heavy investments from the U.S. Government, including the Public Health Department, NASA, Department of Defense, and the Health and Human Sciences Department drove research and innovation in telemedicine. Sending cardiac rhythms during emergencies started at about this time. For instance, in Miami, the university medical center worked together with the fire rescue department by sending electro-cardiac rhythm signals over the voice radio channels from the rescue sites.
One especially successful telemedicine project funded by the government was called the Space Technology Applied to Rural Papago Advanced Health Care (STARPAHC), and was a partnership between NASA and the Indian Health Services. The program funded remote medical services to Native Americans living on the Papago Reservation in Arizona and astronauts in space! Projects like STARPAHC drove research in medical engineering, and helped expand advancements in telemedicine. The next few decades saw continued innovations in telemedicine and wider research at universities, medical centers and research companies.
2. Telemedicine Today
Today the telemedicine field is changing faster than ever before. As technology advances at exponential levels, so does the widespread affordability and accessibility to basic telemedicine tools. For example, not only do we now have the technology for live video telemedicine, but much of the U.S. population has experience using online videochat apps (like Skype or Facetime), and access to a computer or mobile device to use them.
Telemedicine was originally created as a way to treat patients who were located in remote places, far away from local health facilities or in areas of with shortages of medical professionals. While telemedicine is still used today to address these problems, it’s increasingly becoming a tool for convenient medical care. Today’s connected patient wants to waste less time in the waiting room at the doctor, and get immediate care for minor but urgent conditions when they need it.
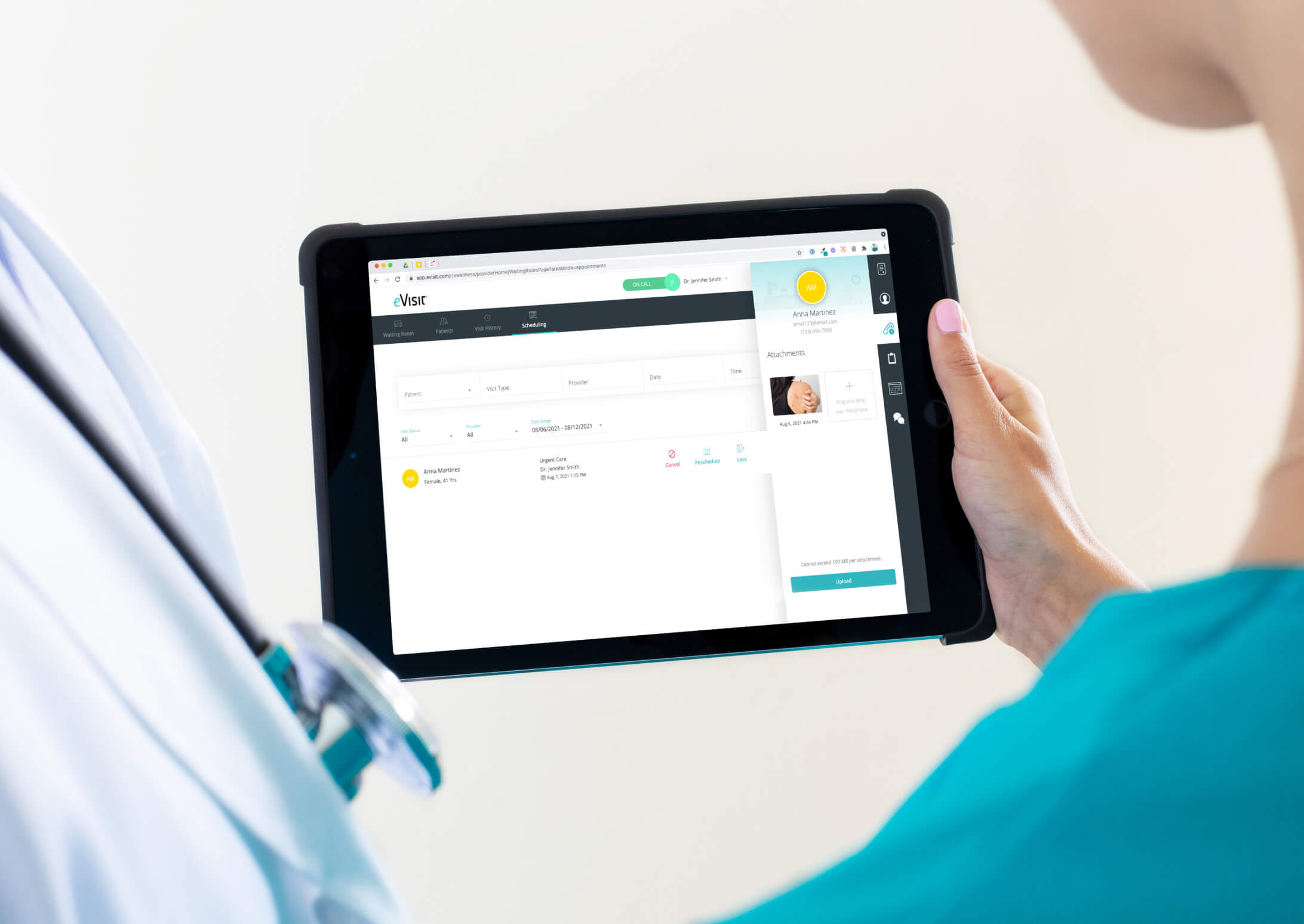
This expectation for more convenient care, combined with the unavailability of many overburdened medical professionals (especially primary care providers) have led to the rise of telemedicine companies. Many offer patients 24/7 access to medical care with an on-call doctor contracted by that company. Others offer hospitals and larger health centers access to extra clinical staff and specialists, for outsourcing of special cases (common model among teleradiology companies). Still others provide a telemedicine platform for physicians to use to offer virtual visits with their own patients. Increasingly, telemedicine is becoming a way to give medical practices an edge in a competitive healthcare landscape where it’s difficult to stay independent or maintain a healthy bottom line.
Also impacting the rise of telemedicine today is the growing mobile health field. With the wide variety of mobile health apps and new mobile medical devices that are consumer-friendly, patients are starting to use technology to monitor and track their health. Simple home-use medical devices that can take vitals and diagnose ear infections, monitor glucose levels, or measure blood pressure let patients gather needed medical information for a doctor’s diagnosis, without going into the doctor’s office. And again, as more patients get proactive about using technology to manage their health, they also will be more open to alternative ways to get care – through telemedicine!
3. Difference between telemedicine and telehealth
With the interrelated fields of mobile health, digital health, health IT, telemedicine all constantly changing with new developments, it’s sometimes difficult to pin down a definition for these terms. In much of the healthcare industry, the terms “telehealth” and “telemedicine” are often used interchangeably. In fact, even the ATA considers them to be interchangeable terms. This isn’t surprising since the telehealth and telemedicine definitions encompass very similar services, including: medical education, e-health patient monitoring, patient consultation via video conferencing, health wireless applications, transmission of image medical reports, and many more.
However, if you want to get technical, telemedicine is really a subset of telehealth. Whereas telehealth is a broad term that includes all health services provided using telecommunications technology, telemedicine refers specifically to clinical services. There’s how the California Telehealth Resource Center defines telehealth:
“Telehealth is a collection of means or methods for enhancing health care, public health, and health education delivery and support using telecommunications technologies.”
Telehealth may involve more general health services, like public health services, whereas telemedicine is a specific kind of telehealth that involves a clinician providing some kind of medical services.
Here are a couple quick examples:
- A public health app that alerts the public of a disease outbreak
- A video-conferencing platform for medical education
Telemedicine:
- A mobile app that lets physicians treat their patients remotely via video-chat
- A software solution that lets primary care providers send patient photos of a rash or mole to a dermatologist at another location for quick diagnosis
As the field of telehealth continues to expand and change, these terms are likely to change and encompass even more health services. Sign up for a telemedicine demo for more insight into the differences.
4. Telemedicine Pros and Cons
In most cases, telemedicine is a net benefit. It expands access to quality patient care, especially to regions and underserved populations that need it the most. It provides a way to cut down on healthcare spending and engage today’s connected patient. It has the potential to change the healthcare delivery model for the better.
However, telemedicine also has a few downsides — by nature of its virtual interaction, and because of societal and technological barriers that could change in the future. The good news is, with the growing popularity and widespread acceptance of telemedicine, we’re likely to see the cons of telemedicine resolve themselves. With new technological advancements and shifting policy that increasingly supports telemedicine, we’re continuously finding ways to improve telemedicine and make it a viable, even advantageous form of healthcare delivery for many medical scenarios.
Here’s a quick overview of the top pros and cons of telemedicine:
Pros of Telemedicine
- More convenient, accessible care for patients
More accessible, convenient healthcare for patients is the driving force behind the telemedicine field. Telemedicine was originally developed in the U.S. as a way to address care shortages, especially in remote rural areas. Now telemedicine is used around the world, whether it’s to provide basic healthcare in third-world countries or allow an elderly patient with mobility issues to see the doctor from home. Telemedicine has the power not only to break down typical geographical barriers to care access, but to make the entire healthcare delivery model more convenient to patients.
- Saves on Healthcare costs
The U.S. spends over $2.9 trillion on healthcare every year, more than any other developed nation. On top of that, an estimated $200 billion of those costs are avoidable, unnecessary spending. Telemedicine has the power to cut our healthcare spending by reducing problems like medication non-adherence and unnecessary ER visits, and making typical doctor visits more efficient.
- Extends access to consults from specialists
With telemedicine, a medical practice or hospital system can immediately expand access to niche medical specialists. This makes it easy for primary care doctors to consult medical specialists on a patient case, and for patients to see a needed specialist on a rare form of cancer, no matter their location. As another example, small hospitals without adequate radiology specialist on-staff can outsource evaluation of x-rays via telemedicine.
- Increasing patient engagement
Today’s patient lives in an increasingly connected world and expects a different kind of care experience. Telemedicine engages patients by allowing them to connect with their doctor more frequently, in a convenient way. That means more questions asked and answered, a stronger doctor-patient relationship, and patients who feel empowered to manage their care.
- Better quality patient care
Telemedicine makes it easier for providers to follow-up with patients and make sure everything is going well. Whether they’re using a more extensive remote patient monitoring system to watch the patient’s heart, or doing a videochat to answer medication questions after a hospital discharge – telemedicine leads to better care outcomes.
For a longer list of the benefits of telemedicine, see Why Telemedicine
Cons
- Requires technical training and equipment
Like most technology solutions, telemedicine platforms usually require some training and equipment purchases. How much is really dependent on the solution – a more extensive inpatient telemedicine platform that will be used between primary doctors and consulting specialist may require more training and the purchase of a telemedicine cart and various mobile health devices. A secure videochat app like eVisit, requires much less staff training and usually only requires purchase of a webcam.
- Some telemedicine models may reduce care continuity
Telemedicine companies that are consumer-facing offer the huge benefit of on-demand care for patients. A sick patient can simply login online and request a visit with one of the telemedicine company’s doctors and get treatment. But this model, similar to the retail health movement, leads to a breakdown in care continuity. A random doctor who doesn’t know the patient, doesn’t know their whole medical history. The best approach to telemedicine? Providing tools to providers to easily connect with their own patients.
- May reduce in-person interactions with doctors
Some critics argue that online telemedicine interactions are impersonal, and physical exams are often necessary to make a full diagnosis. If more patients are resorting to online interactions in place of in-person visits, what effects will that have?
In-person patient-doctor visits are clearly valuable and necessary in many circumstances. Telemedicine is best used to supplement these visits – to do simple check-ins with patients and make sure everything is going well. For minor acute conditions (like infections), an in-person visit with an established patient is often not needed. In those cases, telemedicine can save the patient, the doctor, and the healthcare system time and money.
- Navigating the changing policy and reimbursement landscape can be tricky
Telemedicine reimbursement is a difficult topic, especially with the constantly changing state policies. Many states now have parity laws which require private payers to reimburse for telemedicine visits the same way as in-person visits. The best way to navigate reimbursement is to call up your top payers and ask their policies. You can also check out our guide to telemedicine reimbursement and this helpful matrix from ATA on state policy.
It’s also important to note that many doctors using telemedicine will charge the patient a convenience fee, ranging from $35 – $125 per visit. This fee is direct from the patient and is on top of (or in place of) any reimbursement through a payer. While that means patients are paying out-of-pocket, many of eVisit’s clients have found patients don’t mind, and in fact are happy to pay the additional fee for the convenience.
5. Top Telemedicine Medical Specialties
Telemedicine is used in many different medical fields, throughout ambulatory and hospital settings. Almost every medical field has some use for consulting a patient or another provider (usually a specialist) remotely. Because of shortages of care, limited access to specialists in some areas, and remote locations of patients (especially in rural or sparsely populated areas), telemedicine is incredibly useful to any healthcare provider trying to expand access to quality patient care.
Some medical specialties were early adopters of telemedicine and have pushed development of solutions specifically for their specialty. As a result, there are several key niche telemedicine specialties. Here are some of the most popular telemedicine solutions specialties:
- Teleradiology – Teleradiology is actually one of the earliest fields of telemedicine, beginning in the 1960s. Teleradiology solutions were developed to expand access to diagnosticians of x-rays. Smaller hospitals around the U.S. may not always have a radiologist on staff, or may not have access to one around the clock. That means patients coming into the ER, especially during off-hours, will have to wait for diagnosis. Teleradiology solutions now offer providers at one location to send a patient’s x-rays and records securely to a qualified radiologist at another location, and get a quick consult on the patient’s condition.
- Telepsychiatry – Telepsychiatry allows qualified psychiatrists to provide treatment to patients remotely, expanding access to behavioral health services. Telepsychiatry is incredibly popular, in part because of the nation-wide shortage of available psychiatrists, and because psychiatry often does not require the same physical exams of the medical field.
- Teledermatology – Teledermatology solutions are usually store-and-forward technologies that allow a general healthcare provider to send a patient photo of a rash, a mole, or another skin anomaly, for remote diagnosis. As frontline providers of care, primary care practitioners are often the first medical professionals to spot a potential problem. Teledermatology solutions lets PCPs continue to coordinate a patient’s care, and offer a quick answer on whether further examination is needed from a dermatologist.
- Teleophthalmology – Teleophthalmology solutions allow opthamologists to examine patients’ eyes, or check-in about treatments from a distance. A common example is an opthamologist diagnosing and treating an eye infection. These solutions are usually either live or store-and-forward telemedicine.
- Telenephrology – telenephrology is nephrology practiced at a distance. Telenephrology solutions are most commonly used interprofessionally, when a family physician needs to consult a nephrologist about a patient with kidney disease.
- Teleobstetrics – teleobstetrics allow obstetricians to provide prenatal care from afar. This could mean, for example, recording a baby’s heart at one location and forwarding it to an obstetrician for diagnosis at another facility.
- Teleoncology – the teleoncology field has quickly expanded in the last few years, to provide more accessible and convenient care to patients with cancer. While some teleoncology solutions offer store-and-forward tools to forward images for diagnosis, others are live video platforms to allow patient consults with the oncologist.
- Telepathology – telepathology solutions let pathologists share pathology at a distance for diagnosis, research, and education. Most telepathology tools are store-and-forward solutions, allowing pathologists to share and forward high-resolution images and videos.
- Telerehabilitation – telerehabilitation allow medical professionals to deliver rehab services (such as physical therapy) remotely.
6. What services can be provided by telemedicine
Telemedicine can be used for a wide variety of health services. Here’s a short list of common conditions a primary care doctor may treat via telemedicine:
- Allergies
- Arthritic Pain
- Asthma
- Bronchitis
- Colds and Flu
- Diarrhea
- Infections
- Insect Bites
- Pharyngitis
- Conjunctivitis
- Rashes
- Respiratory Infections
- Sinusitis
- Skin Inflammations
- Cellulitis
- Sore Throats
- Sprains & Strains
- Bladder Infections
- UTIs
- Sports Injuries
- Vomiting
Telemedicine services can range widely by specialty. A surgeon might use telemedicine to do post-operation check-ins with patients, to make sure their wound is not infected. A gynecologist might use a live telemedicine solution to provide birth control counseling. An endocrinologist may do live videochats with patients to discuss recent lab results and answer questions.
The list goes on. If you’re still curious about what services telemedicine is best used for, review this list of Medicare-reimbursed telemedicine services below. It’s by no means a complete list, but it shows you the wide range of health services via telemedicine that are already reimbursable.
7. How does telemedicine work/How can it be used/Types of telemedicine
So by now you know what telemedicine is. But how are telemedicine systems actually delivered? What kinds of technology allows digital connections between a provider at a large hospital and a patient in a remote, rural home?
With the expansion of the internet, much of how telemedicine is delivered has changed. Now, with a simple internet connection, many patients in remote areas can participate in at least some types of telemedicine. Here are a few examples of telemedicine connections.
Networked Programs
Networked connections (like high speed internet lines) are typically used to link remote health clinics to larger health facilities like metropolitan hospitals. According to the ATA, there are about 200 networked telemedicine programs in the U.S., granting telemedicine access to more than 3000 rural sites.
Point–to-point Connections
Point-to-point connections link small remote health centers to one, large, central health facility via high speed internet. This type of telemedicine connection lets smaller or understaffed clinics outsource medical care to specialists at other locations within the same health system. Point-to-point connections are especially common for telepsychiatry, teleradiology, and urgent care services.
Monitoring Center Links
Monitoring center links are used for one type of telemedicine – remote patient monitoring. This type of telemedicine link creates a digital connection between a patient’s house and a remote monitoring facility, so that a patient’s medical data can be measured at home and transmitted electronically to a distant medical monitoring facility. These links usually take the form of internet, SMS, or telephone connections. They’re most commonly used for monitoring of pulmonary, cardiac, or fetal medical data.
8. Types of Telemedicine Consultations
What do you envision when someone says “telemedicine”? The most popular image is probably a doctor consulting a patient via a videochat platform. Two-way video conferencing is quickly becoming a popular virtual alternative to in-person doctor visits.
A telemedicine definition encompasses a much broader range of healthcare services than just real-time medical consultations over video. Telemedicine includes any clinical services provided via telecommunications technology. Here’s a summary of the main types of telemedicine.
Store-and-forward telemedicine solutions
Sometimes called asynchronous telemedicine, store-and-forward solutions enable healthcare providers to forward and share patient medical data (lab results, images, videos, records) with a provider at a different location. These platforms offer a kind of sophisticated, secure, email platform – a way to share private patient data online in a secure way.
The asynchronous term refers to the fact that the consulting specialist, patient, and primary doctor don’t need to all be communicating at the same time. As a parallel, think about a telephone call versus an email exchange. A telephone call (synchronous) requires all parties to be communicating in real-time – an email exchange does not.
Store-and-forward telemedicine works best for interprofessional medical services – where a provider needs to outsource diagnosis to a specialist. For instance, teleradiology relies heavily on store-and-forward technology to allow technicians and healthcare professionals at smaller hospitals to share patient x-rays for diagnosis by a specialist at another location. Asynchronous telemedicine is also commonly used for teledermatology and teleophthalmology.
Store-and-forward telemedicine is a great way to increase healthcare efficiency since a provider, patient, and specialist don’t need to be in the same place, at the same time. It also facilitates faster diagnosis, especially for patients located in underserved settings that may not have the necessary specialist on staff. Overall, this adds up to lower patient wait times, more accessible healthcare, better patient outcomes, and a more optimized schedule for physicians.
Remote patient monitoring
Telemedicine solutions that fall into the remote patient monitoring (RPM) allow healthcare providers to track a patient’s vital signs and other health data from a distance. This makes it easy to watch for warning signs and quickly intervene in patients who are at health-risk or are recovering from a recent surgery, for example. This type of telemedicine is sometimes also called telemonitoring or home telehealth.
RPM telemedicine is quickly rising in popularity as more health professionals realize its potential effects on chronic care management. For instance, a patient with diabetes who has a glucose tracker in their home can measure their glucose levels at regular intervals and transmit them to their doctor. If all is well, those results are simply recorded. If something looks off, the physician may flag it and call in the patient for a consult.
Like most telemedicine tools, remote patient monitoring solutions make it easier for patients and physicians to maintain close communication. Many RPM solutions record and transmit a patient’s medical data automatically, generating a regular report for the physician. In some cases, this medical data is transmitted to a team of health monitoring professionals who are responsible for flagging any warning signs and sending them on to the physician, if needed.
The key to successful remote patient monitoring telemedicine is having the right health tracking tools in the patient’s home. With the recent growth of wearables and mobile medical devices, this is getting easier. Patients have better, cheaper, more accessible tools at their disposal for tracking their health signs and reporting medical data.
Real-time telehealth
Real-time telemedicine (also called “synchronous telemedicine”) is probably what most people first think of when they hear “telemedicine.” Real-time telemedicine requires a live interaction between either a health professional and patient, or between health professionals, using audio and video communication. Think videochat. While most real-time telemedicine software is much more sophisticated than a simple videochat platform, the basic goal is to both see and talk to the patient from afar. This type of telemedicine is meant to offer a virtual alternative to the in-person doctor’s visit.
The popularity of real-time telemedicine solutions has increased rapidly in the past few years, as best telemedicine companies like Teladoc and DoctoronDemand have offered an affordable, easy way for patients to connect with a doctor from anywhere and get immediate treatment.
Doctors are also starting to adopt real-time telemedicine solutions to give their patients the added convenience of virtual doctor visits, improve their care outcomes, boost work-life balance, and reap the many other benefits. With simply a compatible device, internet connection, microphone, and webcam – a patient can now get medical treatment. That’s the beauty of real-time telemedicine.
9. Telemedicine Clinical Guidelines
While the industry is still a long way from a standard set of established guidelines for telemedicine, the American Telemedicine Association has put together guidelines for a range of specialties based on a survey hundreds of research study. What are the clinical, technical, and administrative guidelines a medical practice needs to put in place when they’re adopting telemedicine? Beyond the minimal legal requirements of that state, what are telemedicine best practices?
Based on over 600 studies, the AMA has put together a comprehensive set of guidelines for professionals using telemedicine in primary and urgent care – a field that is quickly adopting telemedicine to expand basic healthcare access. Here are some of the basic protocols and rules a primary care or urgent care facility should put into place when starting their telemedicine program.
When to use telemedicine
While many conditions not on this list can be treated via telemedicine, these conditions are an especially good fit for telemedicine: Allergies and asthma, Chronic bronchitis, Conjunctivitis, UTIs, Low back pain, Otitis media, Rashes, Upper respiratory infections, Diabetes, Hypertension, Mental illness/behavioral health, Prevention and wellness services.
Telemedicine should not be used for any condition where an in-person exam is required because of severe symptoms, certain protocol-driven procedures, or aggressive interventions. Also, for a medical emergency patients should go to the ER or call 911.
Healthcare providers should use their professional judgement to decide when telemedicine is appropriate.
When to prescribe
Prescribing is acceptable for live-video telemedicine sessions, where the visit can substitute for an in-person exam. Prescribing is also ok for telephone consultations, as long as the provider has a pre-existing relationship with the patient.
Informing the patient
Only some states have actually regulations requiring healthcare providers to get patients’ informed consent to use telemedicine. However, this is always good practice, whether or not your state requires it. Before the first telemedicine visit, providers should explain to patients how telemedicine works (when service is available, scheduling, privacy etc), any limits on confidentiality, possibility for technical failure, protocols for contact between virtual visits, prescribing policies, and coordinating care with other health professionals. Everything should be explained in simple, clear language.
Set-up the right space for telemedicine visits
Healthcare providers should create a dedicated space for telemedicine visits to ensure privacy, proper lighting and audio, and avoid interruptions. When possible, providers should place their camera on a level stand and position the camera at eye-level.
Create a contingency plan for emergencies and referrals
Establish a plan for emergencies and communicate it to the patient before the visit. Make sure to have all information on hand for referrals and request transfers.
Patient Management and Evaluation
Always interact with the patient in a culturally competent way, in the language familiar to that patient. If the patient cannot understand because of language barrier, telemedicine should not be used.
It is up to the healthcare provider to use professional judgment to determine when telemedicine is appropriate for the patient case, and when it is not. Also, the patient evaluation should be based on the patient’s medical history and access to their medical record whenever possible.
To guide these decisions, the provider should create clinical protocols which include the condition to be treated (with ICD code), scope of that condition that can be treated using telemedicine, guidelines required to diagnose (when is telephone sufficient, vs. live video), documentation needed to properly assess the patient’s condition, parameters for when the condition can be treated and cannot be treated, and guidelines for when prescription can be done. While this section provides basic, overall guidelines for practicing telemedicine, it’s best practices for the healthcare provider to create more detailed protocols for each condition they intend to treat.
Needed information to diagnose includes:
- Identifying information
- source of the history
- chief complaint
- history of present illness
- associated signs & symptoms
- past medical history
- family history
- personal and social history
- medication review
- allergies
- detailed review of symptoms
- provider-directed patient self-examination (including mobile medical devices if needed)
Quality Assurance
Healthcare providers should do regular quality checks on telemedicine services to identify any potential risks and failures (such as with equipment or connectivity, and patient or provider complaints).
Billing
Providers should inform patients of their cost for service before the visit, whenever possible.
In general, follow the same standards as in-person medical services
Providers should continue to follow the standards they would for any in-person medical visit. For instance, they should practice by the same code of ethics, comply with security guidelines of HIPAA, provide proper documentation to the patient’s primary care provider, follow their licensing and credentialing guidelines.
For more details on guidelines for practicing telemedicine, visit the ATA website.
10. Telemedicine and Medicare
Initially, Medicare only reimbursed providers for very specific health services provided via telemedicine, often with strict requirements. In the past few years with the rapid growth in the telemedicine industry, Medicare has expanded the list of reimbursable telemedicine services but still imposes many restrictions on how the service is provided.
Here are a few things you should know about Medicare and Telemedicine.
- Defining the Originating and Distant Sites. Medicare reimburses for telehealth services offered by a healthcare provider at a distant site, to a Medicare beneficiary (the patient) at an Originating Site. The originating site must be in a HPSA (Health Professional Shortage Area). The types of originating sites authorized by law are:
- physicians or practitioner offices
- Hospitals
- Critical Access Hospitals (CAH)
- Rural Health Clinics
- Federally Qualified Health Centers
- Hospital-based or CAH-based Renal Dialysis Centers
- Skilled Nursing Facilities (SNF)
- Community Mental Health Centers (CMHC).
- Note: Independent Renal Dialysis Facilities are not eligible originating sites.
- The patient must be in a HPSA. In order to be eligible for Medicare reimbursement, the patient (Medicare beneficiary) needs to be receiving virtual care at one of the clinical settings mentioned above, that is also located within a Health Professional Shortage Area (HPSA). To see if the health facility is in a HPSA, use this CMS tool
- Facility Fees. In addition to reimbursement for the telemedicine service, Medicare will pay the originating site a facility fee. For example, if you’re a primary care provider with a patient in your office and you do a telemedicine visit to consult a physician in another location, you could bill for two separate things – the telemedicine service, and a facility fee for using your practice to “host” of the patient visit. Check HCPCS code Q3014 for a full description on facility fees.
- Eligible Providers. Under Medicare, the following healthcare providers can use telemedicine:
-
-
- Physicians
- Nurse Practitioners
- Physician Assistants
- Nurse Midwives
- Clinical nurse specialists
- Clinical Psychologists
- Clinical Social Workers
- Registered dietitians or nutrition professionals
-
- Type of telehealth. Medicare primarily only reimburses for live telemedicine, where the physician and patient are interacting in real-time through secure, videochat. This type of telemedicine visit is meant to substitute a face-to-face in-person visit. The only exception is in Hawaii and Alaska, where Medicare reimburses for store-and-forward telemedicine as well.
- Only certain CPT and HCPCS codes are eligible for telemedicine reimbursement. Medicare has a specific list of CPT and HCPCS codes that are covered under telemedicine services. Since that list is subject to change each year, we recommend you also periodically check the CMS website for the most up-to-date codes.
- When billing, use the GT modifier. When billing for telemedicine visits, you need to include the “GT” modifier with the relevant CPT code to indicate the service was provided virtually.
Find out the Medicare reimbursement rates. Curious what Medicare will reimburse for a telemedicine visit? Use the Medicare Physician Fee Schedule Lookup tool to type in your code and check rates based on your location.
11. Telemedicine and Medicaid
Unlike with Medicare, Medicaid programs are state-run and therefore subject to state law on telemedicine practice. That means telemedicine reimbursement through Medicaid is widely dependent on what the policy is in your state.
Based on the Center for Connected Health Policy’s recent report, here’s a quick overview of what Medicaid reimbursement for telemedicine looks like across the U.S.:
- 46 states Medicaid programs cover live video
- 9 state Medicaid programs will cover store-and-forward telemedicine
- 14 state Medicaid programs cover remote patient monitoring
- Only 3 state Medicaid programs (AK, MN, MS) offer coverage for all three types of telemedicine
- 26 state Medicaid programs cover a facility or transmission fee, or both.
So, where do you start the research process? We have 3 reliable sources we use to track Medicaid coverage of telemedicine:
- The National Telehealth Policy Resource Center. Check out their fantastic interactive map of telehealth policy, state-by-state.
- Visit your state Medicaid agency website. Here’s a full directory if you don’t have the website handy.
- The American Telemedicine Association. The ATA does regular telemedicine policy updates, and releases quarterly reports on the state telemedicine legislation landscape. Check out the latest report here.
Factors that Affect Medicaid Reimbursement for Telemedicine
Since telemedicine requirements vary by state and aren’t always 100% clear, it’s good to know what to look for. Here is a quick list of the factors you should note, that could affect your telemedicine reimbursement through Medicaid.
- Health Services covered
- Eligible providers (NPs, PAs)
- Is cross-state medical licensing allowed?
- Is a pre-existing relationship with patient required?
- Location restrictions on patient or provider
- Applicable CPT codes
- Type of fee reimbursed (transmission, facility, or both)
12. Future of Telemedicine
There’s a lot to be optimistic about in the future of telemedicine. With rapid advances in technology, it’s likely that telemedicine will only become easier and more widely accepted in the coming years. Already, smart glasses (like Google Glass) and smart watches (like the Apple Watch) can monitor patients’ health data and transmit them in real time to health professionals. Programs like clmtrackr can analyze a person’s emotional state based on their facial expressions and could be used to monitor mental wellness. Digital health startups like Augmedix, are experimenting with automatically transcribing documentation during a patient visit. Advances in robotic surgeries allow surgeons to operate on patients from afar.
To keep up with the rate that technology is progressing, the telemedicine will of course need to overcome other administrative barriers, such as restrictions placed on telemedicine practice by state legislation, state-specific licensing requirements by medical boards, and the reimbursement policies that affect whether doctors are reimbursed by payers and patients are not out-of-pocket. But with the projection that telemedicine will be a $36.3 billion industry by 2020, over 50 telehealth-related bills in the 113th Congress, and 75% of surveyed patients reporting interest in telemedicine, telemedicine’s future is bright and demand is likely to overcome these barriers.
13. Telemedicine Statistics
With all the claims about the benefits of telemedicine, it seems to be a no-brainer. But what is the research telling us about telemedicine? What do the statistics and findings about telemedicine really show?
All the numbers point to the exponential growth of telemedicine – in other words, it’s not going anywhere. The global telemedicine market was worth $17.8 billion in 2014, and is projected to grow well beyond that by 2020. ATA President Dr. Reed Tuckson estimated that approximately 800,000 virtual consultations will take place in the U.S. in 2015. And health systems, doctors, legislators, and patients are fueling that upward trend. A recent survey found an incredible90% of healthcare executives were in the process of developing or implementing a telemedicine program, and 84% said these program were important. IHS projected the number of patients using telemedicine will rise from roughly 350,000 in 2013 to 7 million by 2018. And with this high demand for telemedicine, legislators are scrambling to pass bills that offer both support and needed regulations; in August 2015, Congress had 26 telemedicine-related bills waiting for decision.
The telemedicine foundation is quickly being built. But what do patients think about telemedicine? Are they ready to try it? Recent studies show that a majority of patients are interested in using telehealth services, especially once they see how telemedicine works and the potential benefits for them. NTT Data found 74% of surveyed US patients were open to using telemedicine services, and were comfortable communicating with their doctors via technology. 67% said telemedicine at least somewhat increases their satisfaction with medical care.
While the loss of an in-person human interaction is often cited by skeptics of telemedicine, 76% of patients said they care more about access to healthcare than having an in-person interaction with their doctors. Also, only 16% if surveyed patients would rather go to the ER for minor conditions if they could instead use telemedicine for treatment. With the ongoing shortage of patient slots open with overburdened primary care doctors, these stat says a lot about patients’ willingness to try out telemedicine.
While widespread research on the effects of telemedicine is still relatively young, many studies do show positive results. When the Veterans Health Administration implemented telemedicine for past heart attack patients, they sawhospital readmissions due to heart failure drop by 51%. Another study on the Geisinger Health Plan showed that telemedicine reduced 30-day hospital readmissions by as much as 44%. And while telemedicine skeptics often claim virtual visits tend to be lower quality than in-person visits, a recent study of 8,000 patients who used telemedicine recorded no difference in care outcomes between in-person and virtual care.
There’s a lot to be optimistic about telemedicine. A survey of healthcare executives found improving the quality of patient care was their top reason for implementing telemedicine and in another study, respondents said the top benefit was ability to provide round-the-clock care. About half of patients also reported that telemedicine increases their involvement in treatment decisions, getting them engaged in managing their care. And with a potential $6 billion per yearthat US employers could save by offering telemedicine to employees, telemedicine can have a huge impact reaching past the healthcare industry.
14. Telehealth Resource Centers
The United States has 14 Telehealth Resource Centers, all funded by the U.S. Department of Health and Human Services’ Health Resources and Services Administration (HRSA) Office for the Advancement of Telehealth. These resource centers serve as a local hub of information and research about telehealth, usually with a focus on increasing healthcare access for underserved communities. Plus, the services they provide are generally free!
While all the telehealth resource centers offer helpful information about navigating telehealth, each center has specific strengths. Here’s a quick overview of the top centers to check out as you’re getting started with telehealth.
For a listing of all centers or to find your regional center, check out the Telehealth Resource Center site.
National Telehealth Policy Resource Center
Phone: 877.707.7172
Direct: 916.285.1860
- Check out their interactive U.S. map of telehealth policy, state-by-state
- You can follow them on Twitter, Facebook, or by email to get regular provide telemedicine news and policy updates.
- Excellent resources section with fact sheets, policy briefs, and even a micro-documentary on telemedicine!
California Telehealth Resource Center
Phone: 877.590.8144
- Great page on best practices for developing a telemedicine program
- Sample forms and guidelines to use in your telemedicine program
- Training page with links to webinars, videos, and free on-site training services for California programs
Heartland Telehealth Resource Center
Phone: 877.643.HTRC (4872)
- Excellent reimbursement guides for Kansas, Missouri, and Oklahoma
- Comprehensive, up-to-date regulation guides for Kansas, Missouri, and Oklahoma
Mid-Atlantic Telehealth Resource Center
Phone: 855.MATRC4U (628.7248)
Direct: 434.906.4960
- State-specific resources for Virginia, West Virginia, Kentucky, Maryland, Delaware, North Carolina, Pennsylvania, Washington DC, and New Jersey
- Request a speaker on telemedicine
- Directory to find telehealth providers
National Telehealth Technology Assessment Resource Center
Phone: 877.885.5672
Direct: 907.729.4703
A great resource for anyone looking for technology and devices to integrate into a telemedicine program.
- Toolkits on new technologies, medical devices, and apps to use with your telemedicine program
- User Reviews section on different telehealth technology and devices
NorthEast Telehealth Resource Center
Phone: 800.379.2021
- Great Telehealth “A to Z” section with resources organized into categories such as clinical, financial, and technology
- Telehealth toolkits for psychiatry and dermatology
15. Telemedicine Regulations
Telemedicine regulations are in constant flux as medical associations (like the FSMB and AMA) continue to develop basic guidelines for telemedicine practice, and states introduce new legislation to enact telemedicine policy.
Telemedicine regulations also determine the telemedicine reimbursement rules followed by Medicaid and private payers in that state. With the explosion of new telemedicine companies and patient demand for virtual care, the number of telemedicine-related legislation currently on the table is at an all-time high. Most U.S. states have passed new telemedicine regulations recently, or have a proposed bill awaiting decision.
Consequently, telemedicine regulations can vary widely from state-to-state in these key areas.
Parity Laws
Currently, 29 states and the District of Columbia have passed telemedicine parity laws. A telemedicine parity law requires private payers to reimburse for telemedicine, though the specific restrictions on reimbursement often vary by state. In many cases, private payers reimburse for the same amount as the comparable in-person medical service.
Parity laws also may affect coverage by the state Medicaid program.
Cross-state licensing
One of the key advantages of telemedicine is the ability to provide healthcare to a patient, no matter the patient or provider’s location. However, since providers are licensed to practice in a specific state, they are only legally allowed to offer telemedicine services to patients in the same state. Currently, 49 state medical boards require physicians practicing telemedicine to be licensed in the state where the patient is located.
Cross-state licensing would allow providers to provide care to a patient in a nearby state, without holding a full license to practice in that state. Some states are moving to pass measures to allow state medical boards to work together and establish cross-licensing requirements.
Patient Informed Consent
Some states require providers to get a patient’s informed consent for telemedicine services. Some regulations require written consent, others require verbal, or none at all. Either way, it’s good practice for providers to inform patients about telemedicine services and what to expect.
Online Prescribing
Most states have specific regulations on which medications can be eprescribed and which cannot. For the most part, schedule III to V drugs can be prescribed online. But many schedule II drugs (commonly used for chronic pain management) cannot be prescribed via telemedicine services, as regulations require an in-person exam.
Pre-existing Physician-patient relationship
In many states, current regulations require that any provider and patient doing a telemedicine visit have a pre-existing relationship. Usually this means that the provider and patient need to have had at least one in-person visit. This regulation is slowly changing as more companies like Teladoc and DoctoronDemand seek to connect patients with a random, on-call doctor for immediate care.
Resources
Want to learn more about telemedicine legislation? Here are the sites we use to stay up-to-date:
- The National Telehealth Policy Resource Center
- Visit your state Medicaid agency website
- American Telemedicine Association state legislation matrix
16. Barriers to Telemedicine
While the field of telemedicine has taken off in the past few years, there are still barriers to widespread adoption.
Legislation
State legislation determines the restrictions and often, the reimbursement rates for telemedicine services administered in that state. For instance, any state that has passed a telemedicine parity law has mandated that private payers in that state to reimburse telemedicine visits at the same rate as a comparable in-person visit. While a majority of states have now passed telemedicine parity laws, changing state legislation is often a time-consuming, unwieldy process and can have a huge impact on the telemedicine practices in that state.
Reimbursement process
Reimbursement for telemedicine services is often not as straightforward for traditional medical services. State telemedicine policy landscape is continuously shifting, affecting rules around reimbursement through state Medicaid programs and through private payers. Medicare does now reimburses for real-time telemedicine services, but places restrictions on the eligible healthcare providers, the location of the patient, the medical procedures that can be done, etc. The good news is, there is a shift towards more widespread reimbursement for telemedicine through all third-party payers, with less restrictions.
Implementation/Equipment costs
The growth in telemedicine solutions means that telemedicine options are now more diverse, with many more affordable solutions. However, most telemedicine programs do require the purchase, set-up and staff training of new technology and equipment – some of which may be outside the budget of providers in smaller independent practices. Many providers are already stretched thin on new technology budgets and staff training for EHR systems, imposed by the Meaningful Use program. Also, for patients who may not have access to a smartphone or a computer with internet, real-time telemedicine may be out of reach.
State Licensing requirements
Healthcare providers currently earn their medical licenses for a specific state. This lets them practice medicine legally in that state, and only that state. This presents a problem for telemedicine, as the entire goal is to break down geographical barriers between a patient and provider. According to medical licensing regulations, a specialist based in Colorado would not be legally allowed to treat a patient in New Mexico.
In response to this barrier, some telemedicine groups and providers have started pushing for cross-state medical licensing.
17. Who Pays for Telemedicine
Medicare
Medicare pays for telemedicine services under certain circumstances. Primarily, Medicare covers live telemedicine services, or virtual visits delivered via interactive audio and video (think videochat). The goal is to cover medical services delivered virtually where an in-person visit may be difficult for the patient or provider. Store-and-forward telemedicine services are only covered in Hawaii and Alaska at this time.
Additionally, Medicare will only pay for telemedicine services when the patient is located in a Health Professional Shortage Area and receives care from an eligible provider. The medical service itself also has to fall under one of thesecovered CPT/HCPCS codes. When all these conditions are met, Medicare pays for 80% of the physician fee (other 20% is paid by the patient) and will additionally pay a facility fee to the originating site.
Medicaid
Medicaid will cover telemedicine services depending on the legislation passed in that state. Since Medicaid programs are state-run, they follow state-specific telemedicine regulations. In 46 states, Medicaid offers some kind of physician reimbursement for telemedicine services delivered over live video. 26 state Medicaid programs will also pay an additional facility or transmission fee to cover the cost of hosting a telemedicine visit, or transmitting patient medical data in a secure way. The specific restrictions and regulations around telemedicine vary widely by state. To find out more about you’re your state Medicaid program will cover, visit the Center for Connected Health Policy’s recent report.
Private Payers
Private payers are increasingly paying for telemedicine services based on popular demand and evidence of cost-savings from virtual care. For instance, United Healthcare recently announced it would expand coverage for 24/7 on-demand virtual visits to people enrolled in employer health plans.
How does telemedicine work and which telemedicine services private payers pay for again can vary widely by state. While the trend is toward broader coverage of telemedicine services for plan enrollees, private payers are still deciding on exactly what they will cover and what they won’t. 29 states and Washington, DC have passed telemedicine parity laws, which mandate that private payers in those states pay for telemedicine services at the same rate as in-person visits.
Patients
In many cases, telemedicine visits are actually paid by patients directly. Online services that offer patients 24/7 on-demand access to a virtual doctor will often charge a per-visit fee or a monthly or yearly subscription for access. Those charges are not billed through insurance and come directly out of the patient’s pocket.
Many doctors who choose to offer virtual visits to their patients will do so as part of a direct-pay or concierge practice model. Instead of having their doctor bill through an insurance carrier, these patients might have a high-deductible insurance plan for emergencies and then pay a yearly fee to essentially have their doctor on retainer. The patients might pay an additional convenience fee for each virtual visit, or just have access to virtual visits with their doctor as part of their subscription fee for the practice.
18. HIPAA and Telemedicine
Like all technology in the healthcare space, telemedicine solutions need to be HIPAA compliant to protect patient privacy. While an app like Skype might offer a doctor an easy way to consult a patient remotely, using it in that way is not in compliance with HIPAA. Technology used for telemedicine services needs to ensure high-level security and prevent any breaches of patient personal health data.
But as the National Policy Telehealth Resource Center notes, “Compliance with the Health Insurance Portability and Accountability Act (HIPAA) is more complex than simply using products that claim to be ‘HIPAA-compliant.” Not only does the telemedicine platform need to be compliant, all providers, patients, and staff using the tool need to ensure they are in compliance with HIPAA. A telemedicine software vendor, for instance, not only needs to build a secure product, but also ensure their telemedicine company is operating in accordance with HIPAA.
HIPAA compliance entails an organized set of secure, monitored, and documented practices within and between covered entities. Though products cannot ensure compliance, some products may contain elements or features that allow them to be operated in a HIPAA-compliant way.
19. Telemedicine And Telehealth Terminology
The following are some of the most commonly used definitions and terms that are used in telehealth and telemedicine.
Application Service Provider (ASP): Various applications are hosted by an ASP on a central server. Customers can pay a fee to access the applications they want to use over either a private network or secure Internet connection. This allows customers to rent applications that they need to use from an ASP instead of having to buy, install and then maintain software on their own. Usually software upgrades and new releases are included in the rental price.
Asynchronous: Sometimes this term is used for describing the process of store and forward transmission for sending information or medical images since typically the transmission takes place in one direction, as opposed to synchronous which transmits in both directions.
Authentication: This is a method that is used to verify an individual’s identity who is receiving or sending information. Keys, passwords or another type of automated identifier is used for the verification.
Bandwidth: Measures a communications channel’s information carrying capacity; for a telemedicine service, this is a practical limit to its capabilities, cost and size.
Bluetooth Wireless: Bluetooth refers to an industrial specification that applies to wireless area networks. Bluetooth technology offers a way of connecting and exchanging information between devices, including laptops, mobile phones, PCs, video game consoles, digital cameras and printers over a globally unlicensed and secure short-range radio frequency. The Bluetooth Special Interest Groups has developed and licensed the Bluetooth specifications.
Broadband: Communications (e.g. satellite, microwave and broadcast television) that has the capability to carry a wide range of various frequencies; it refers to signals being transmitted in a frequency-modulated manner, over a portion of the total available bandwidth, which permits several messages to be transmitted simultaneously.
Clinical Information System: Exclusively relates to information concerning patient care, as opposed to administrative data. It is a hospital-based information system that has been designed for the collection and organization of data.
CODEC: This is an acronym for coder-decoder. It is a videoconferencing device (e.g., Panasonic, Sony, Tandberg, Polycom, etc) that converts analog audio and video signals into audio and digital video code and vice versa. Typically CODECs compress digital code in order to conserve a telecommunication path’s bandwidth.
Compressed video: In order to send information over a phone network, video images often need to be processed in order to reduce how much bandwidth is needed for capturing the required information.
Computer-based Patient Record (CPR): Individual patient information in electronic format that has been designed to provide access to accurate and complete patient information.
Data Compression: A method that is use for reducing the volume of data. Encoding is used to reduce storage space requirements, bandwidth requirements, transmission times and image processing. Some information loss make take place with some compression techniques, this might be clinically important or not, depending on the specific circumstances.
Diagnostic Equipment: (Cameras, Scope and Other Types Of Peripheral Devices): A hardware device that is separate from a central computer (e.g. camera, stethoscope or digitizers) that can offer medical data input into a computer or accept output from one.
Digital Camera: Typically used for taking still images of patients. Some of the general uses that this kind of camera is used for include wound care and dermatology. The images that this type of camera produces can be download onto to a PC and then sent over a network to a consultant or provider.
Digital Imaging and Communications in Medicine (DICOM): This is a communications standard for medical imaging devices; it is a set of protocols that are vendor-independent and describe how to identify and format images. It was developed by the National Electronic Manufacturers Association and American College of Radiology.
Disease Management: A coordinated and continuous health process for the purposes of managing and improving the health status of a specifically defined population of patients over the complete course of the disease (e.g., DM, CHF). The targeted patient populations are high-cost, high-risk patients that have chronic conditions that require appropriate care in order to be maintained properly.
Distance Learning: The use of audio and video technologies allows students to attend training sessions classes that are conducted from a remote location. Usually distance learning systems are interactive. They are a useful tool for delivering education and training to students that are widely dispersed, or in some cases where an instructor is unable to travel to the site where the students are located.
Distant Site: Refers to a telehealth site where a specialist or provider either consults with the patient’s provide or see the patient from a distance. Other common names that are used for this term include referral site, physician site, provider site, specialty site, consulting site and hub site.
Document Camera: This type of camera is able to display type or written information (e.g., lab results), graphics (e.g. ECG strips), photographs, and x-rays in some cases.
Electronic Data Interchange (EDI): Directly receiving and sending data between two trading partners without human invention or paper.
Electronic Patient Record: Individual patient information in electronic format which provides access to accurate and complete patient data, links to medical information, clinical decision support systems, reminders, alerts and other types of aids.
Encryption: A system for encoding data on an email or web page where only the computer system or person authorized to access the information can retrieve and decode it.
Firewall: Computer software and hardware that blocks unauthorized communications between external networks and an organization’s computer network.
Full-motion Video: Refers to a standard video signal which makes it possible for video to be displayed at a distance in uninterrupted, smooth images.
Guideline: A procedure or policy statement for determining a course o action or providing guidance on setting standards.
H.320: A technical standard pertaining to videoconferencing compression standards which enables various equipment to interoperate via IDSN or T1 connections.
H.323: A technical standard pertaining to videoconferencing compression standards which make it possible for various equipment to interoperating using Internet Protocol.
H.324: A technical standard pertaining to videoconferencing compression standards which make it possible for various equipment to interoperate through using Plain Old Telephone Service (POTS).
HL-7 (Health Level-7 Data Communications Protocol): A communication standard guiding health-related information transmission. HL-7 allows various applications to be integrated into one system, including patient accounting, order entries, hospital census, radiological imaging stations, and bedside terminals.
HIPAA: Health Information Portability Act acronym.
Home Health Care And Remote Monitoring Systems: Care that is provided to patients and their families in their residences to promote, maintain or restore health; or to minimize the effects of illness and disability, including terminal illnesses. In Medicare enrollment data and claims as well a Medicare Current Beneficiary Survey, home health care is defined as home visits made by professionals, including physicians, nurses, home health aides, therapist and social workers. The use of interactive devices and remote monitoring enable a patient’s vital signs to be sent on a regular basis to health care providers without the patient having to travel.
Informatics: Utilizing information technologies and computer science in order to process and manage knowledge, information and data.
Integrated Services Digital Network (ISDN): A common dial-up transmission path used for videoconferencing. ISDN services are on demand services where another IDSN based device is dialed, and per minuted charges are accumulated at a certain contracted rate. The site that places the call is then billed. The service is similar to the dialing features that come with making long distance phone calls. The person how initiates the call pays the bill. Connections of up to 128Kbps are permitted by ISDN.
Interactive Television/Video: Similar to video conferencing technologies that make is possible for synchronous, two-way interactive audio and video signals to be transmitted for delivering distance education, telemedicine or telehealth services. The acronyms are often used to refer to it- VTC (video teleconference), IATV or ITV.
Internet Protocol (IP): The protocol for sending data from one computer over the Internet to another. Every computer that is on the Internet has one address at least that identifies it uniquely from all of the other computers that are on the Internet. Internet Protocol is a connectionless form of protocol, meaning there isn’t a connection that is established between the two points that are communicating with one another. A videoconferencing system’s IP address is its telephone number.
Interoperability: This refers to two systems ((software, networks, communication devices, computers and other types of information technology components))or more being able to interact with each other and exchange information so that predictable results can be achieved. There are three different kinds of interoperability: technical; clinical and human/operational.
ISDN Basic Rate Interface (BRI): A type of ISDN interface that provides 128K of bandwith tht is used for videoconferencing as well as simultaneous data and voice services. A multiplexer can be used to link together multiple BRI lines in order for higher bandwidth levels to be achieved. For example, one popular option among telehealth networks is combining 3 BRI lines in order for video-conferencing to be provided with 384K of bandwidth. BRI services are unavailable in some rural areas. Before videoconferencing equipment is order for using this kind of service, one needs to check with their telecommunications provider to see if BRI services are available.
ISDN Primary Rate Interface (PRI): An ISDN interface standard which operates using one 64K data channel and 23, 64K channels. When the right multiplexing equipment is used, the user can selected the IDN PRI channels for a video call. As an example, if a user would like to have his videoconference at 384K bandwidth, the multiplexer can be instructed to utilize channels 1-6 (6 x 64k= 384k). It is actually quite importance since usually the user pays charges that are based on how many 64k channels get used on a videoconference. So the fewer channels that have to be used to get a quality video signal, the lower the cost of the call will be.
JCAHO – This is an acronym for Joint Commission on Accreditation of Healthcare Organizations.
Lossless – This is a kind of data compression which allows users to reconstruct images without losing the information from the original copies. It can achieve a compression ratio 2:1 for images with color.
Lossy – This is a process of compressing data with high ratio. The unnecessary information are discarded when reconstructing the images.
Nursing Call Center – This is a centralized office where nurses are the ones who are working. The nurses are responsible for answering telephone calls from patients. They should also make responses to faxes, electronic mails and letters from patients. Nursing call centers may also provide the callers with the basic information regarding their health, but they should not disclose the diagnosis made by the doctors on their conditions. They should not prescribe medications as well. They may just provide basic instructions when patients are having health complaints.
Mobile Telehealth Clinic – This involves using vehicles like van, trailer or any mobile unit to provide health care services for patients. The services are given by health care professionals. This is helpful to those who are living on areas far from the hospital. Some mobile units are equipped with medical technologies that are found in the hospital like mobile CT, MRI and TeleDentistry.
Multiplexer or MUX – This is a device that chooses several digital inputs and combines them into a to be transmitted on a single line.
Multi-point Control Unit or MCU – This is a device used to connect a few videoconferencing sites into a single system. Multi-point Control Unit is also referred to as the “bridge”.
Multi-point Teleconferencing – This is the process of connecting multiple users from different sites. It allows electronic communication between the users as well as transmission of video, voice and data between computers and systems. Multi-point teleconferencing requires the use of a multi-point control unit or the bridge to be able to connect the different sites for the videoconference.
Network Integrators – These are the organizations that give services and develop software to allow sharing of data, videos and voices and communication between different devices and systems.
Originating Site – This is where the patient and physician are located during the time of consultation. This site is also called as patient site, remote site, spoke site or rural site. This allows the patients to access their personal health information from anywhere with the help of the Internet.
Patient Exam Cameras – These cameras are used to examine the patient’s overall condition. The different types of patient exam cameras are handheld cameras, camcorders, gooseneck cameras and those which may be placed above the set-top units. Analog and digital cameras are available and the ones that should be used depend on the connection to the set-top unit.
Peripheral Device – This is a device that can be connected to the computer. Examples of peripheral devices include mouse pointers, keyboards, video camera, scanner and monitors used for clinic and hospitals including weight scales and pulse oximeters.
Telepharmacy Solutions – This refers to the provision of pharmacy services to the patients with the use of communication technology and electronic information. This is used when the patients cannot go personally to avail such services.
POTS – This is the acronym for Plain Old Telephone Service.
Presenters or Patient Presenters – They are the ones who provide telehealth services and perform the overall exam for patients. Such presenters should be on the medical field and they must have experiences in providing health services to patients like registered nurses and licensed practical nurses. They were trained in the use of the equipment like cameras and computers, and they are the ones who communicate with the patients on the originating site. They can also perform the different activities which are part of the diagnostic examination.
Regional Health Information Organization/Health Information Exchange (RHIO/HIE) – These are the organizations that ensure the quality, efficiency and safety of the health services delivered by the Telehealth.
Router – This is a device which provides connection to at least two networks on an organization. It provides network connection on multiple locations and it is responsible in finding the best route between two sites. It tells the videoconferencing devices where the destination devices can be found and it will find the best way to gather the information from that specific destination.
Standard – This term refers to the benchmark used to measure the quality of the results. The standard is established by the authority to make sure that organizations are achieving the desired results.
Store and Forward – This is a form of telehealth consultation which uses images from the patients to come up with the medical diagnosis. The different types of Store and Forward services include dermatology, radiology and wound care. It may also include transferring of patients’ clinical data like ECG and blood test results from the patients’ site to the hospital’s site.
Switch – In the videoconferencing world, switch refers to the device responsible for selecting the path that will be used in transmitting the video. It is similar to an intelligent hub and it can direct traffic on hub ports to different destinations. The hub ports will then feed the devices with the same information.
Synchronous – This term refers to the interactive connections between two videos when the information are transmitted at the same time for both directions.
System Integration – This involves bringing together two systems and devices and sharing data and information between the two systems.
T1/DS1 – This is a type of service for telephone lines that provides a bandwidth data service of 1.544 Mbps.
T3/DS3 – This is a carrier that allows the users to have a bandwidth data service of up to 45 Mbps.
Transmission Control Protocol/Internet Protocol – This involves the standard rules for establishing and maintaining network conversation between two computers with the help of the Internet.
Telecommunications Providers – These are the entities authorized by the U.S. government to provide telecommunications services to all residents and institutions in the U.S.
Telemedicine/Telehealth: Basically, these two terms are used to describe the use of technology and telecommunications to exchange medical information from one place to another with an aim of improving the patient’s health status. Telemedicine is sometimes involved in direct patient clinical services which include diagnosis and treatment of patients.
Teleconferencing : This is the interaction between multiple users across various sites with the use of interactive electronic communication. This involves transfer of video and audio through computer and video systems. This interaction is usually live and is mostly used in the diagnosis or monitoring a patient in home care.
However, there are other terms that fall under telecommunication in health care. They are:
1. Telementoring- which is basically the use of video, audio and other electronic and telecommunication processing technologies to offer individual guidance. A good example of this would be a physician mentoring a local healthcare provider who is new in the healthcare industry.
2. Telemonitoring- this is process of using video, audio and other electronic and telecommunication systems to transfer live information between computers with an aim of monitoring the health status of a patient from a distance. A good example would be home care.
Telematics : This is the integration or use of information processing that is based on a computer, and using telecommunications to allow programs and data transfer between computers.
Telepresence : Technically, this is the use of robotics and other technologies to allow a medical practitioner to perform a procedure at a certain location by using devices and receiving sensory information or feedback which contributes to a sense of presence and allowing certain achievement in a procedure.
A good example would be the utilization of lasers or even hand pieces as well as receiving pressure that is equal or similar to that created by physical hands. This gives the perception of presence, thus achieving a satisfactory degree of achievement.
Teleradiology : This is the transfer of radiological images. X-Rays, MRIs and CTs are all types of radiological images. These images are used for consultation, diagnosis or interpretation. They can be transferred through satellite connections, local area networks or even standard telephone lines. The Picture Archiving and Communications Systems allow centralized storage and the access of these images over information systems such as computers.
Universal Service Administrative Company: Abbreviated as USAC, the Universal Service Administrative Company is responsible for administering USFs or Universal Service Funds to allow easy access to telecommunication services across the country. The Rural Health Care Division which is under USAC as well manages discount programs for telecommunications health care.
Ultrasound Device : This is any device that employs high frequency sound technology to examine internal body organs. These devices are used to detect tumors and other inner body organs abnormalities.
WiFi : Wifi was originally licensed but the Wi-Fi alliance and it is used to describe the technology of wireless local area networks, abbreviated as WLAN. This technology was primarily developed for mobile computing devices like laptops in Local Area Networks, but with technological advancements, it is now used for an array of services which include VoIP phone access, gaming as well as basic connection of electronics such as smartphones, DVD players, Home theaters and Televisions.
Videoconferencing Systems: This is equipment and software that allows real time two way communication, which is usually in the form of digitized audio and video. These systems are mainly used for meetings without necessary having to be in the same room. Each individual needs equipment that can send and receive audio and visual information.
Only certain CPT and HCPCS codes are eligible for telemedicine reimbursement
Check this list for the eligible CPT/HCPCS codes. CMS updates this list on a yearly basis. The code will need to accurately describe the medical service provided via telemedicine.
When billing, you’ll need to use the GT modifier
In addition to the right CPT or HCPCS code, you’ll need to use the “GT” modifier when billing to show that the service was delivered via telemedicine. If you’re a provider located in Hawaii or Alaska using a store-and-forward telemedicine solution, use the GQ modifier instead.
Only certain providers can get reimbursed for telemedicine
Here’s the list of eligible providers:
Physicians
Nurse Practitioners
Physician Assistants
Nurse Midwives
Clinical nurse specialists
Clinical Psychologists
Clinical Social Workers
Registered dietitians or nutrition professionals
The originating Site can also charge a facility fee
Since the originating site is essentially hosting the telemedicine visit, Medicare allows the originating site to bill a separate facility fee. For more details on the facility fee, look up HCPCS code Q3014.
Medicare reimburses telemedicine at the same rate as a comparable in-person visit
Whether you’re billing a 99213 that was done in-person or via telemedicine, your billable rate should match the standard Medicare physician fee schedule ($72.81). Want to check the Medicare physician rates? Lookup reimbursement rates for any code here.
Medicare Advantage plans have much more flexibility than traditional Medicare!
All the guidelines and restrictions we’ve listed above are for billing telemedicine through traditional Medicare. Medicare Advantage plans under a commercial payer have complete flexibility to cover telemedicine however they want! This means, Advantage plans may cover telemedicine for your patient and not have any of those restrictions on what qualifies as an eligible originating site. Call the payer and ask what they’ll cover and what their telemedicine guidelines are.
The future of Medicare & Telemedicine
What’s likely to change in the coming years? It’s hard to say, but Medicare’s coverage of telemedicine seems to expand every year.
On July 7th, 2015, House representatives introduced the Medicare Telehealth Parity Act of 2015. If passed, the bill will expand what telemedicine services Medicare will cover and get rid of many limitations (like the requirements for what qualifies as an “originating site“). Legislation like this one could have a huge impact on coverage for remote patient monitoring and other telemedicine services delivered to the patient in their own home.
Other helpful resources on Medicare and telemedicine
Want more information? Check out our Top 10 FAQs about Medicare & Telemedicine top 10 FAQs and our complete guide to Telemedicine Reimbursement.